Factors Associated with Acute Kidney Injury and Mortality During Cardiac Surgery
Background
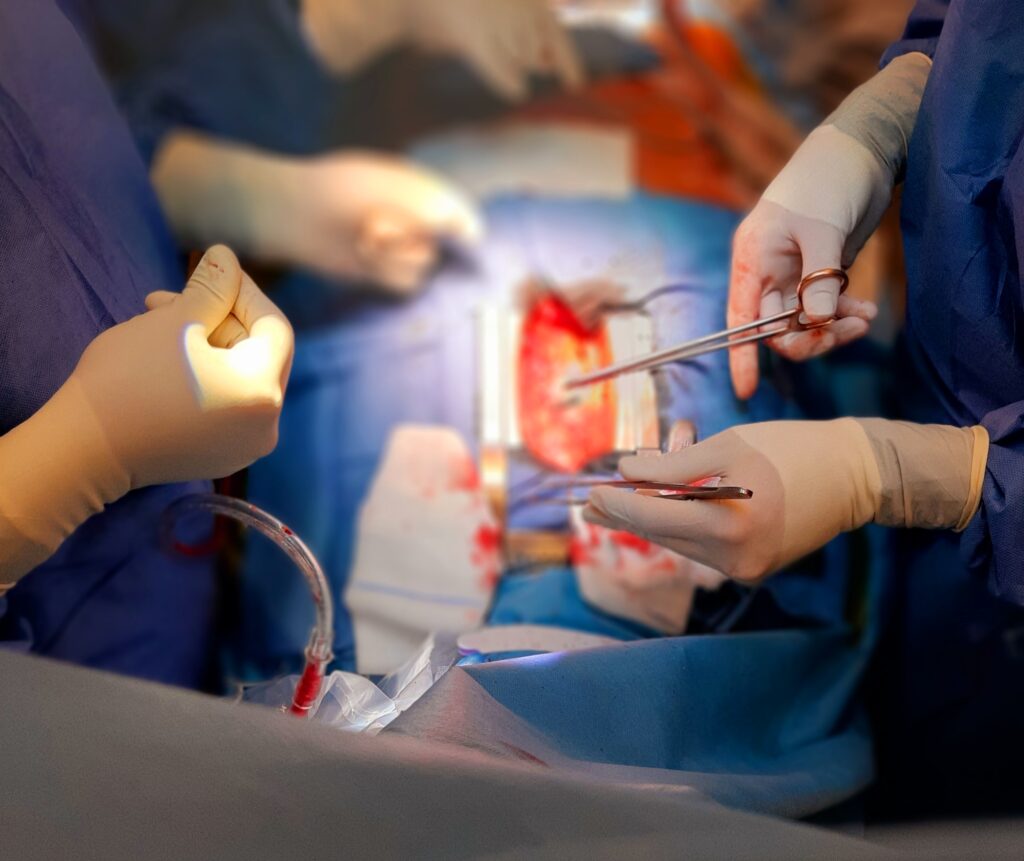
Cardiac surgery with cardiopulmonary bypass (CPB) is known to contribute towards the incidence of acute kidney injury (AKI) and peri-operative morbidity and mortality. There are several patient, anaesthetic and surgical factors that contribute to its occurrence. It is imperative to know the profile of a patient who is likely to develop this complication to mitigate for modifiable risks. This study aimed at describing a profile of AKI in an adult patient (over the age of 18 years) following cardiac surgery on CPB. Factors associated with the development of cardiac surgery-associated acute kidney injury (CSA-AKI) are described, as well as the relationship between CSA-AKI and in-hospital mortality.
Methods
This was a contextual, descriptive and retrospective single-centre study with data of 476 adult patients admitted post cardiac surgery between January 2016 and December 2017. Data were collected from Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) in South Africa. All adult patients who presented for elective cardiac surgery (coronary artery bypass graft), valvular, aortic and other cardiac surgery on CPB were included. Peri-operative factors such as patient demographics, baseline renal function, co-morbid factors, length of CPB and aortic cross-clamp time, degree of hypothermia, use of assist devices, and post-operative serum
creatinine (SCr) levels were collected. Incomplete essential peri-operative data and data for patients who presented on renal replacement therapy (RRT) already were excluded. AKI was defined by Kidney Disease Improving Global Outcomes (KDIGO) criteria.
Results
One hundred and thirty-five (28%) patients developed CSA-AKI and 20, 5 and 3% were in KDIGO 1, 2 and 3, respectively. Older age (p = 0.024), female gender (p = 0.015), higher serum creatinine level (p = 0.025), and lower estimated glomerular filtration rate (eGFR) (p = 0.025) were associated
with the development of CSA-AKI, while a history of hypertension was predictive. Forty-six of the 476 patients died. Mortality rates were significantly higher in those with AKI compared to those without [28 (21%) vs 18 (5%), respectively (p = 0.001)]. The incidence was significantly worse in those with severe kidney injury, as evidenced by mortality rates of 44 versus 5% between KDIGO 3 and KDIGO 1 (p < 0.001). Pre-operative eGF and CSA-AKI requiring RRT were significantly associated with mortality, while pre-operative eGFR was an independent predictor of mortality (hazard ratio 0.99, 95% confidence interval: 0.97–0.99, p = 0.019).
Conclusion
A history of hypertension was predictive of the development of CSA-AKI, and preoperative eGFR was an independent predictor of mortality in this cohort. Both factors are modifiable.
