COVID-19 and ECMO: An Unhappy Marriage of Endothelial Dysfunction and Hemostatic Derangements
Severe respiratory syndrome coronavirus-2 is responsible for coronavirus disease 2019 (COVID-19), which may lead to acute respiratory failure. In its most severe manifestation including refractory hypoxemia and/or hypercapnia, it can require escalation to extracorporeal membrane oxygenation (ECMO). Rates of thromboembolic complications are elevated in COVID-19 patients despite deployment of thromboprophylaxis.
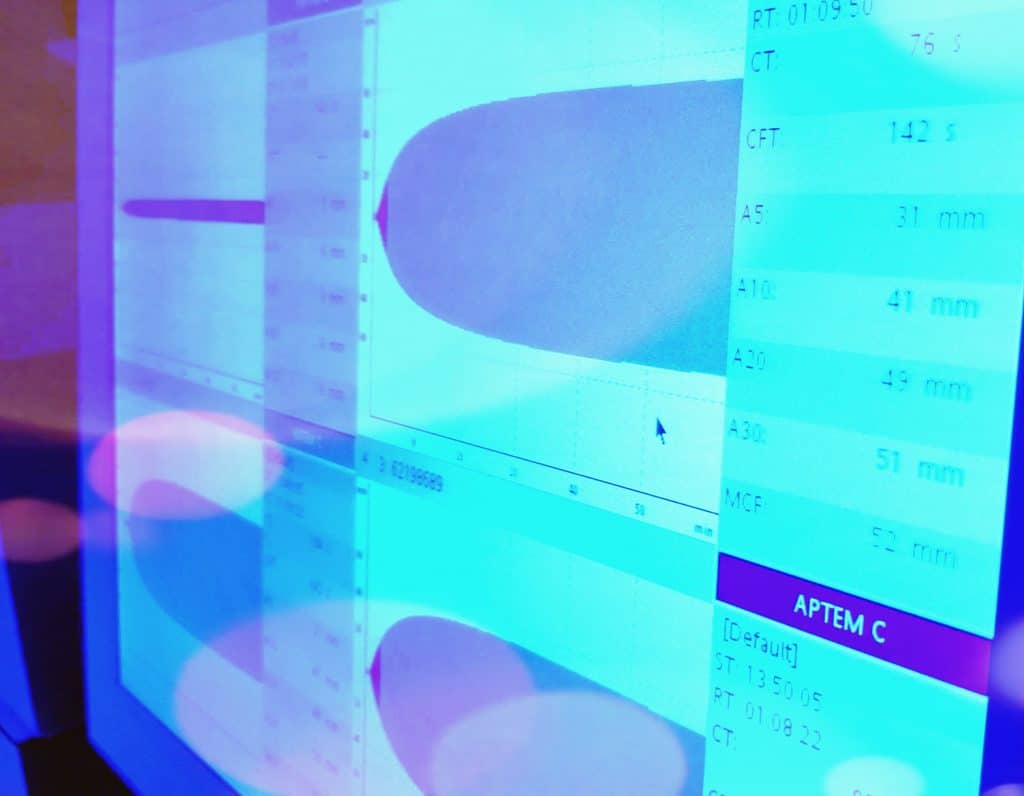
Among the sickest COVID-19 patients requiring ECMO, much less is known regarding hemostatic derangements, as well as the resulting risk profile for the development of both thromboembolic and hemorrhagic complications. Thus, defining the ideal pharmacologic anticoagulant approach (agent, intensity, monitoring) for these critically ill patients remains a challenge. A recent case series by Usman et al. highlighted safety issues encountered in a cohort of 10 COVID-19 patients cannulated for venovenous ECMO (VV-ECMO) and subsequently anticoagulated with unfractionated heparin (three patients) or argatroban (one patient).
Of these, Usman et al. reported hemorrhagic strokes in four patients despite modest activated partial thromboplastin time (aPTT) reflective of typical levels of anticoagulation for maintenance of mechanical support (mean aPTT without stroke 41.8 seconds v 52.8 seconds with stroke, p = 0.09) and, in all affected individuals, platelet counts greater than 130,000 per µL with fibrinogen counts >250 mg/dL. Similarly, systolic blood pressures appeared largely within normal limits preceding the diagnosis of intracranial hemorrhage (ICH). ICH in COVID-19 previously has been reported with a yet-to-be determined incidence or underlying etiology.
