PERFUSIONIST: The LAYMAN’s Approach

“Perfusion is a profession that has a very low public profile. It is reputed to be one of the most stressful lines of work a person could possibly choose.“
Author / Editor:
Co-Editor Anna Lou Villena 🙂
[12]
According to the American Society of Extracorporeal Technology: Perfusion is a profession that has a very low public profile. It is reputed to be one of the most stressful lines of work a person could possibly choose. In fact, by way of benchmarking, it is placed in the same category as air traffic controllers and nuclear facility engineers. The latter profession sounds more sophisticated but these professions share a common element, and that is – the ever present possibility that when a mistake is committed, it might be accompanied by catastrophic consequences.
In the limelight of Cardiovascular surgery, Perfusionist is a medical professional, educated and trained in the science of Extracorporeal circulation who works closely with Cardiovascular and Thoracic surgeons and anesthesiologists in the delivery of care, primarily to the cardiac surgical patients. The Perfusionist is trained in physiologic principles and techniques to maintain homeostasis and must be knowledgeable and skilled in the conduct of extracorporeal circulation to ensure safe management during operative procedure.
In LAYMAN’s Approach
Beyond the dogma of medicine, Perfusionist should be cognizant. Mr. Martin Fisher thought that “The practice of medicine is a thinker’s art, the practice of surgery a plumber’s.” More so, the perfusionist’s side chain of responsibility runs the gamut from TIMEKEEPing and PLUMBing.
The TIMEKEEPER
=
A timekeeper records time, time taken or time remaining during a certain event. In parallel, the perfusionist records important data and time tracking during the course of the operation. The surgeon, anesthesiologist and circulating nurses rely on our time record. Significantly, surgeons randomly ask us to keep them posted with their speed, get tracked on the precision of our execution or just plainly test our presence of mind if we didn’t forget to press the timer when bypass was initiated (***wink).
Specifically, we keep track of the following common parameters:
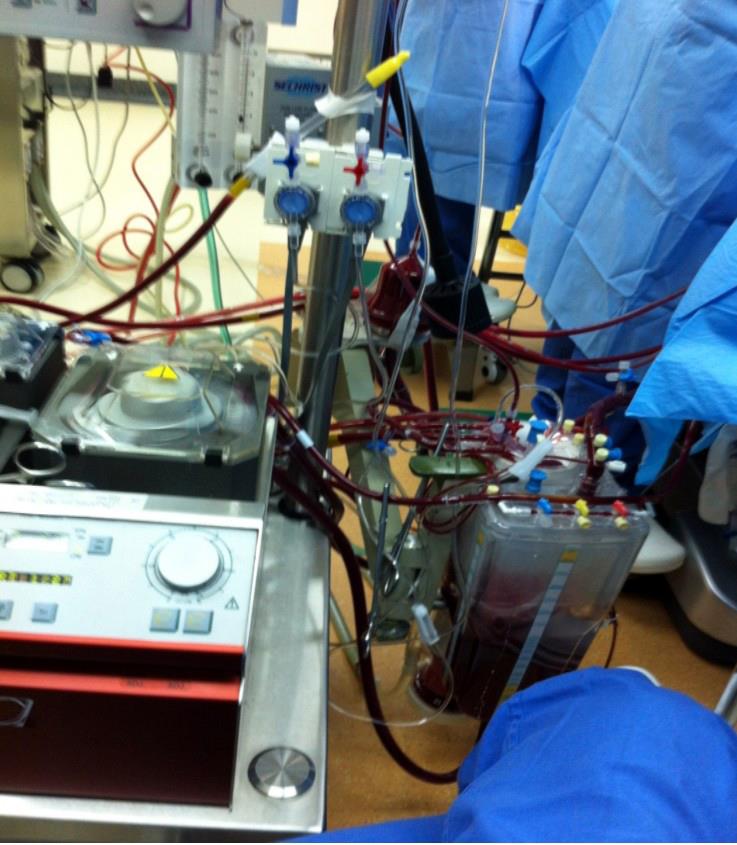
- Bypass time – from bypass initiation where heart lung machine starts to run, venous blood drains from right atrium or from superior/ inferior vena cava to the reservoir, pumped in an accurate flow rate by a roller or centrifugal pump, going to the membrane oxygenator, passing through an arterial filter and oxygenated blood goes in the aorta. Time ends when blood volume is returned to the patient by gradually clamping or occluding the venous tube and eventually perfusionist/surgeon signals OFF Pump.
- Ischemic time – starts when the cross clamp is applied to the aorta and separate the systemic circulation from the outflow of the heart, wherein adequate perfusion flow from the heart lung machine physiologically maintains the systemic vital organs while the heart is temporarily arrested using a cardioplegia solution in the form of pure crystalloid or a combination of patients own blood and crystalloid solution. Time ends when the aortic cross clamp is removed while patient is placed in a Trendelenburg position (head down).
- Cardioplegia time – starts when the first induction dose of cardioplegia solution following cross clamping is completely given. Intermittent dose interval time vary according to the surgeon’s preference. Some prefer it to be given every after 20 minutes, others every after 30 minutes and some even preferred to be given continuously. Some surgeons are often reminded when it’s time to give cardioplegia in order to uphold myocardial protection and others just command according to their own discretion.
- Rewarming time – the surgeon signals when it is time to start rewarming usually initiated when the surgical procedure is near completion. Typically, rewarming is done slowly following a norm of 3 minutes per degree increment. The temperature of the water in the heat exchanger versus the patient’s blood temperature should not go beyond 42°C and a gradient of 12°C in an adult and 8°C in pediatric patient. During rewarming, the patient’s blood flow rates and FiO2 are increased at incremental rates because the solubility of oxygen is decreased and the metabolic oxygen demand of the patient increases.
- Reperfusion time – starts after the aortic cross clamp is released, thus oxygenated blood flows in the heart after a period of temporary ischemia. Some surgeons prefer reperfusion time to be 1/3 of the ischemic time before heart is allowed to eject.
- MUF (Modified Ultrafiltration) Time – starts after termination of cardiopulmonary bypass (CPB) to remove excess water from the patient and to salvage blood from the bypass circuit. Some perfusion practice make a fixed MUF time of 10 minutes as their endpoint while others do a hematocrit analysis and determines the endpoint if hematocrit value reaches 28-30%.
Indeed simple responsibilities greatly affect the chronology of the whole pump run reminding us that TIME has its own reason and everything doesn’t just happen at once.
The PLUMBER
The plumbers are known for their ingenuity and resourcefulness. They are mostly adventurer who traces leaky pipes to their source. Relatively, the perfusion tool box carries the same thing.
When the operating theater is flooding due to water leaks or disconnected hose from the heater-cooler machine, the perfusionist takes the action and responsibility. Definitely, in the same wavelength the perfusionist or a plumber prevents or puts an end to leaks of sensitive information.
In its complexity, the arterial – venous circuit is designed to permit the maximum calculated blood flow rate without excessive line pressures from resistance. Adequate venous drainage should be achieved without shunting to the right heart while eliminating the need or minimizing blood product requirements.
Perhaps, Perfusionist also deals with pipes = tubings and couplings = connectors ranging from different sizes measuring the diameter in inches (3/16, ¼, 3/8 and ½) and also comes in a variety of shapes (straight and “Y”). All mentioned are used according to patient’s needs and case specificity, thus configuring the integrity of the PIPELINE = CIRCUITRY.